Genentech
Optimal Patient Pathway Study
Mapping lived experiences of IPF patients
Genentech, a biotechnology company sought to gain insight into the experiences patients diagnosed with Idiopathic Pulmonary Fibrosis (IPF) face in their care delivery journeys.
Objectives & Approach
A qualitative study aimed to shed light on the journey faced by patients with Idiopathic Pulmonary Fibrosis (IPF) and their caregiving loved ones. Along with a second researcher, I conducted in-depth, semi-structured interviews in patients’ homes to explore gaps in care during the path to diagnosis, through disease management, and into end-of-life planning.
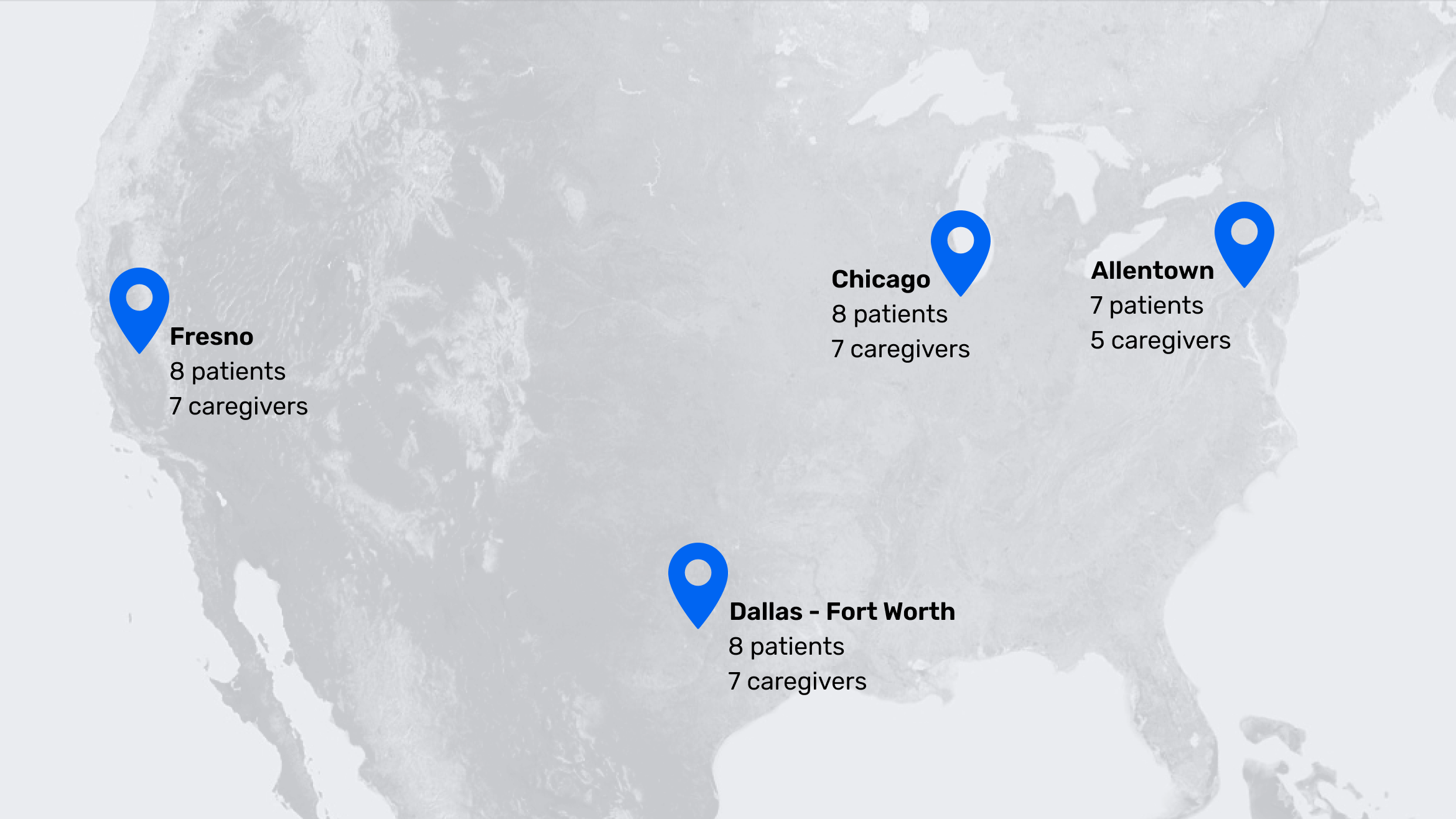
Geographic Context
Study participants were recruited from four distinct regions, spanning both rural and urban communities. This deliberate mix allowed us to capture regional variations in attitudes and access to Interstitial Lung Disease Centers of Excellence.
Personal, Not Just Clinical, Insights
An interview guide supported exploration of patient’s experience from pre-diagnosis through ways of living with and treating the disease. Included, were discussions of end-of-life considerations for patients not to pursuing lung transplant as a treatment option.
Methods
This study illuminated the human impact of IPF. Understanding the deeply personal mental models of patients and their familial caregivers as the disease progressed was crucial.
In Home Visits
Interviewing IPF patients in their homes alongside their caregivers and families provided a deeper understanding of how they navigate the daily challenges of their condition. I witnessed firsthand the creative adjustments they made to their living spaces—like rearranging furniture for easier movement and setting up oxygen equipment—and heard moving stories about the emotional and practical support systems that have become essential to their ongoing care. These conversations highlighted not only the resilience of patients and families but also the importance of adapting both routines and environments to meet the evolving demands of the disease.
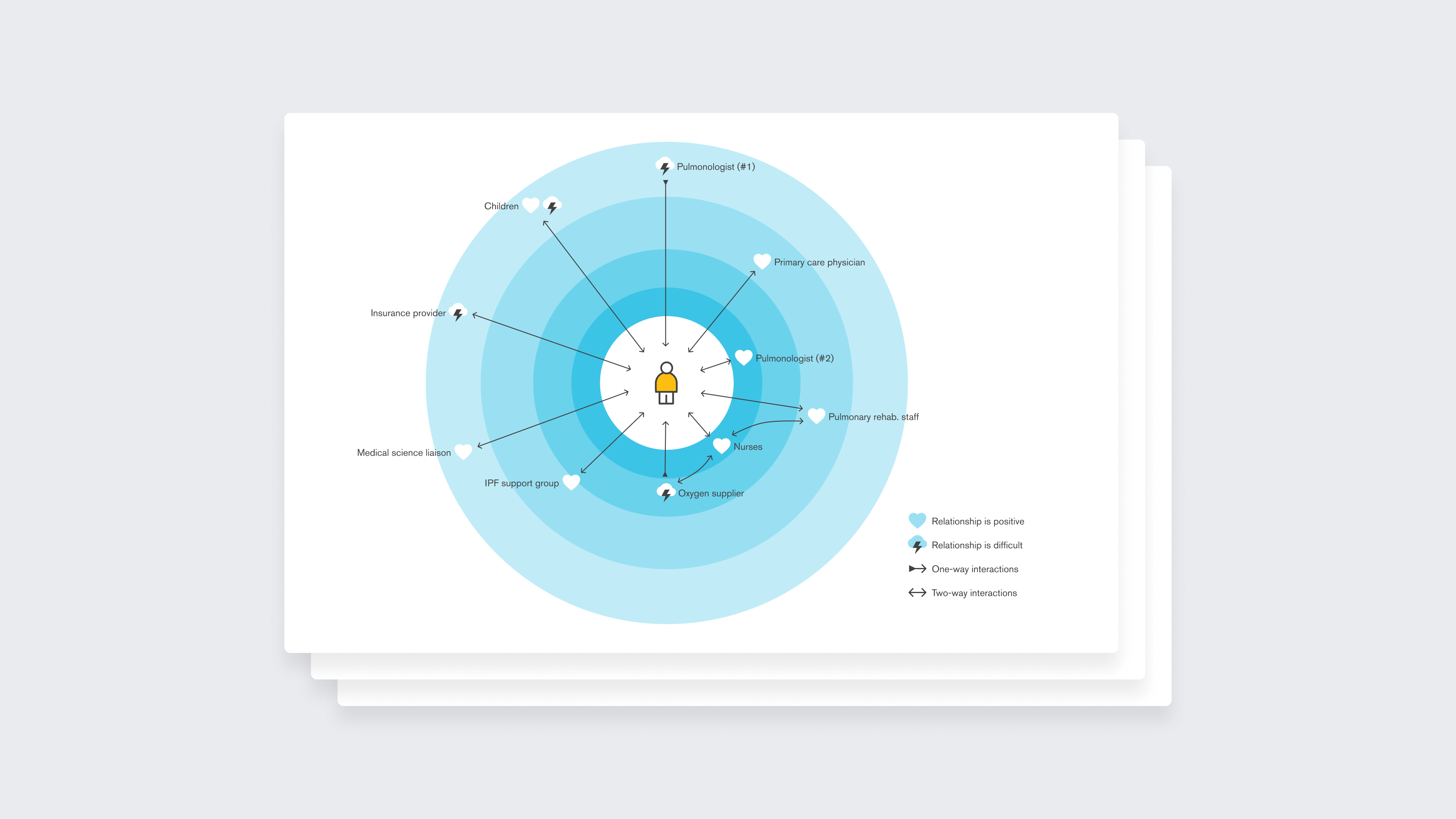
Circles of Care
At the end of each interview, patients participated in a collaborative mapping exercise to identify key relationships and individuals involved in their care. The exercise helped to illustrate patterns of positive support and points of friction throughout their IPF experience.
Findings & Insights
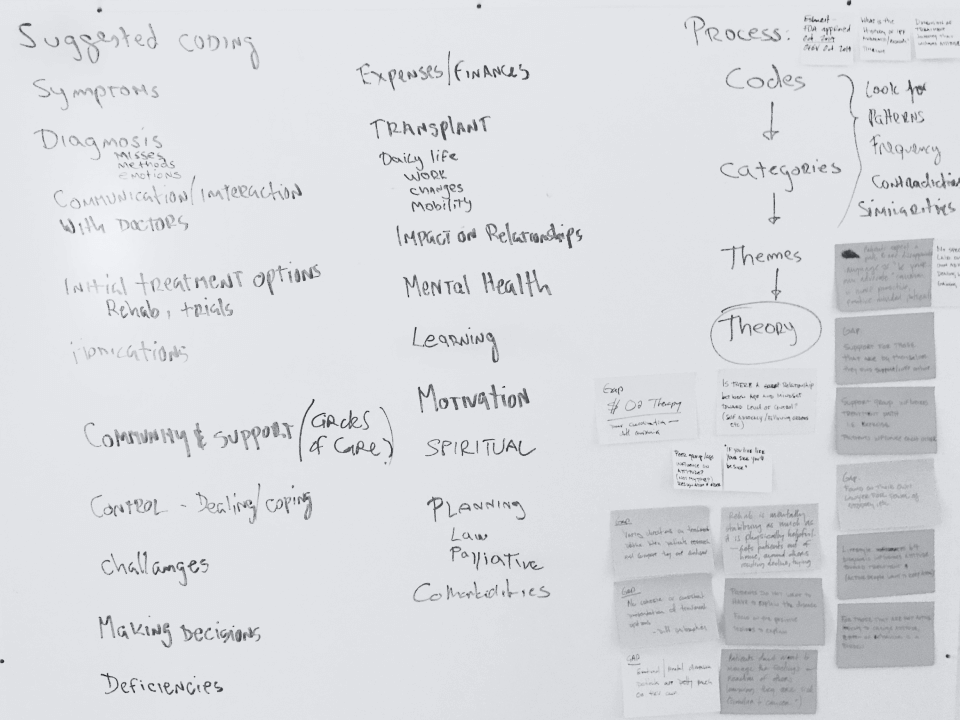
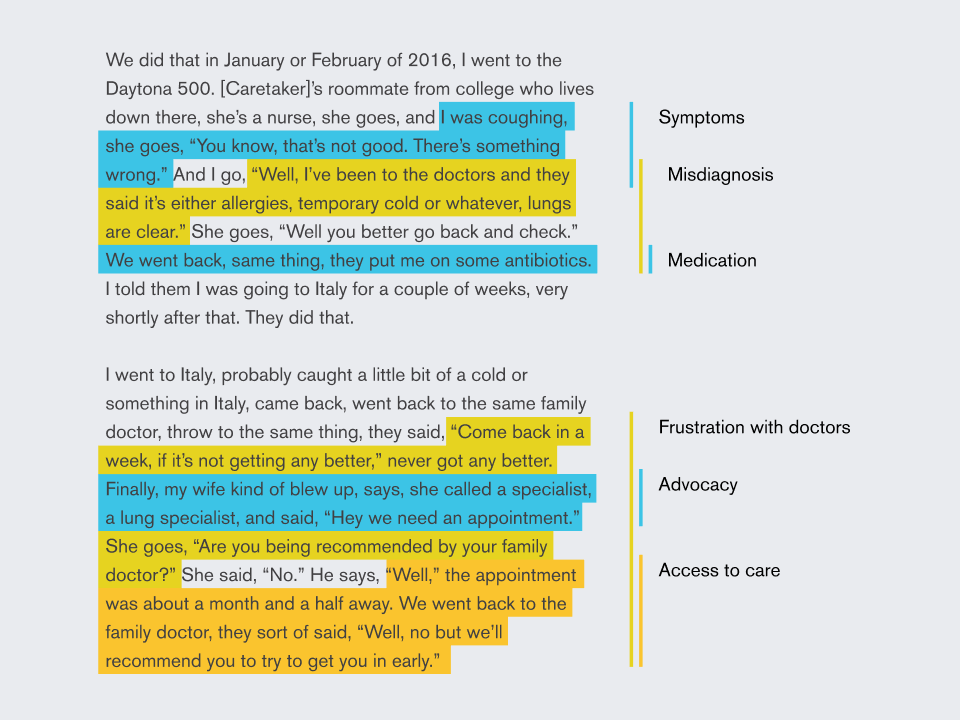
Unpacking, organizing, and transforming raw conversations into findings that summarized patient's experiences of seeking an accurate medical diagnosis and the outcomes associated with receiving one.
To organize and make sense of the the hours of interview transcripts we used coding to explore and identify themes, the frequency of occurrences, and the relationships between different codes.
“I’ve just felt like I’ve been flying by the seat of my pants, you know. Stuff happens and you think ‘okay, well is that because of the disease, is that because of the medication?’”
– Jackie, age 74
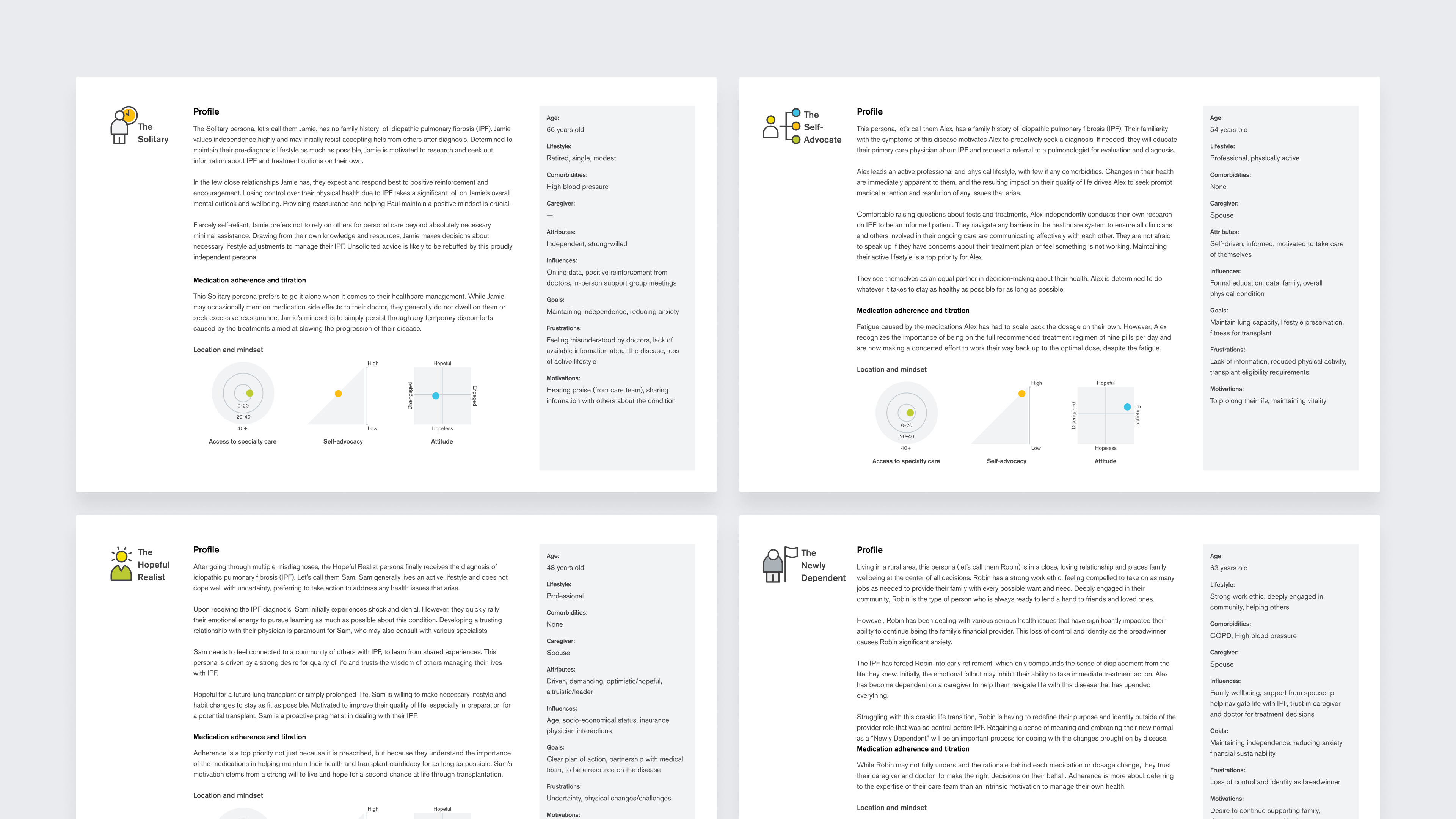
To build empathy, we personified the struggles, emotions, and pivotal decisions faced by patients and their caregivers. This approach allowed our sponsors to better understand the personal experiences underlying their clinical data.
Personas
We created four distinct patient personas and one for their caregiver. Each captured a combination of demographics, psychographics, and situational factors that influence an IPF patient's journey.
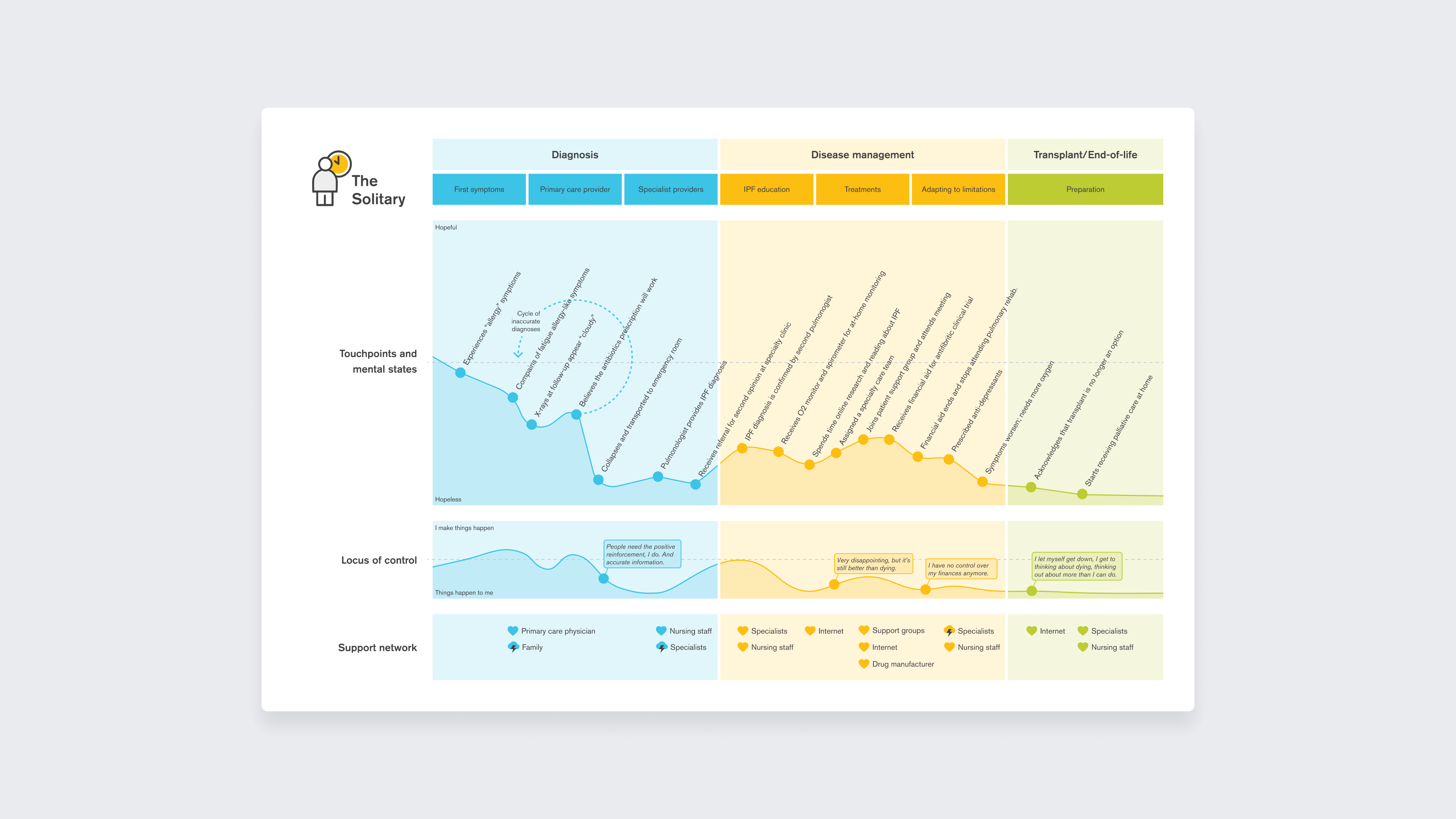
Journey Maps
Comprehensive journey maps were then created for each persona, documenting their pathways from initial symptom onset, through their process to proper diagnosis, into disease management, and finally to transplantation or end-of-life care planning.
Summary
The research revealed that patients with Idiopathic Pulmonary Fibrosis (IPF) face a range of challenges throughout their care journey.
Through their stories, we documented how these issues create uncertainty and frustration, damaging trust in medical providers and straining relationships at home. The findings point to several urgent needs and opportunities for clearer information, better support systems, and more standardized care pathways to help IPF patients and their families.
Observations
Lack of education about this rare disease, difficulty in establishing the diagnosis, resource constraints, overwhelming demands on health care providers, referral and consultation challenges (including geography), and uncertainty about best practices for diagnosis and management are only a few of the problems.
Patients are willing to try antifibrotics which are discordant from the views that patients unwilling because of quality-of-life issues.
Patients had positive experiences with the multidisciplinary teams available during their lung transplant evaluation.
Patients feel positive when they attend IPF support groups and receive valuable clinical information about IPF and treatments.
Opportunities
Grass roots education of primary care physicians, community health workers, nurses, and radiologists; telemedicine for health care providers and radiologists; and public disease awareness campaigns to improve the patient journey.
Introducing an IPF team (with social workers) early on after a working diagnosis.
Training, guidelines, and funding from the Pulmonary Fibrosis Foundation to standardize care for IPF patients, especially at ILD centers of excellence.